Home/Articles
/ General Dental /
Reena’s Notes: WORNing Tooth Wear Ahead! 10 Key Points with Professor Andrew Eder
June 29, 2021
- In 1968, 37% of the UK population had no teeth. Contrastingly in 2009, 6% have no teeth. Within this group, caries and periodontal disease rates have fallen but tooth wear is increasing as people are living and keeping their teeth for longer (ADHS 2009). Other factors that have contributed to the increase in tooth wear burden including a change in diet. For example, the consumption of soft drinks have increased from 13.6 billion litres in 2008 to 14.8 billion in 2014 (energy drinks have doubled). Currently, the majority of the population (75% adults, >50% children) have tooth wear. National guidelines exist for the prevention of dental caries and periodontal diseases. GDC also has placed an emphasis on oral cancer detection. However, there are no clear guidance on monitoring and preventing tooth wear despite it having a growing societal impact from a health and financial perspective).
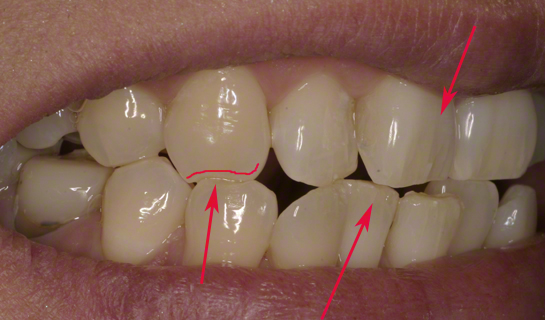
- Early recognition is key but we don’t always see what we are not looking for so it’s important to have a proactive approach. Note down the sites (teeth, surfaces) affected as well as the extent (enamel, dentine) and severity (mild/moderate/severe). It can also be helpful to distinguish between physiological and pathological tooth wear, as this will influence your management.
- Determine the aetiology(ies) – abrasion, attrition, erosion, abfraction. It is normally multi-factorial. Then identify the cause(s) – i.e. what is causing the tooth wear. This is also normally multi-factorial and it may help to think outside the box.
- Look out for the markers of tooth wear. Physical markers: hypertrophic masseters, buccal keratosis, cheek biting, scalloping of the tongue, loss of canine guidance and wear facets. Medical markers: xerostomia, sleep disorders aggravating parafunction and stomach acid regurgitation. Social markers: alcohol misuse, caffeine as it encourages parafunctional activity, erosive diet, recreational drug use, intense sporting activities and sport-induced dry-mouth and sports drinks. Identifying these will help identify a holistic approach to management.
- Monitor tooth wear through study casts (digital recording may be useful in the future), photographs, putty indices and tooth wear indices. The first two are the most reliable. The BEWE (Basic Erosive Wear Examination) by Bartlett et al 2008 provides criteria for the grading of erosive wear which then guide management.
- Definitive treatment for tooth wear should ideally follow compliance and stability. Treatment may range from the provision of a Michigan splint, to composite build-ups or full mouth rehabilitation.
- Know when to refer cases – this may depend on the level of complexity as well as challenges such as the lack of space.
- Multifactorial risk assessment models for other multi-factorial diseases exist e.g. for caries – Cariogram by Malmo University. There is a need for risk assessment tool for tooth wear e.g. Wearogram
- The clinician and patient need to be aware that tooth wear is a lifelong challenge from a monitoring, treatment and maintenance perspective.
- Further reading: Worning: Tooth Wear Ahead: PDJ 2016:5(3)38-42.
Learn more by reading some of our other articles here.



