Home/Articles
/ General Dental /
Reena’s Notes: Endodontics vs. Implants with Dr Peter Briggs – 23 Key points providing an Evidence-Based Overview
March 23, 2016
Introduction
- What do patients prefer? Evidence on patient-centred outcomes show similar levels of satisfaction for both treatment modalities i.e. saving a tooth with root canal treatment and post versus extraction and replacement with an implant-retained crown (Gatten et al 2011). There is no advantage from a patient’s perspective of an implant crown over a restored root-treated tooth if the aesthetics are similar. Patients are generally very satisfied with fixed replacement options however they are delivered.
- Experience and formal training affect dentists’ decision-making according to Lang-Hua 2014. Dentists with formal implant training tend to preserve more teeth than those with non-formal training. They also tend to do less posterior implants (they go that extra mile to save posterior teeth – probably due to the greater risks associated with posterior teeth) and place less implants per space than those with non-formal training.
Comparing Survival
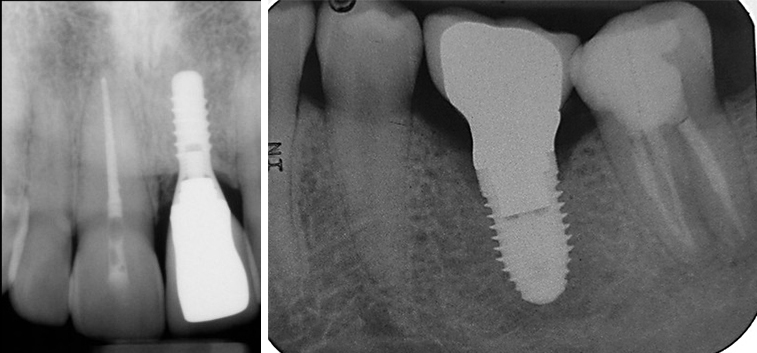
- When comparing survival rates, these are similar for endodontically treated teeth and implant-retained crowns. However, implants require a significantly greater amount of intervention, which can vary from connective tissue graft and remedial surgery for peri-implantitis to screw loosening (Doyle et al 2006).
- Tooth survival for endodontically treated teeth at 8-10 years was 87% in the Ng et al 2010 study. Positive influential factors in order of significance: a full coverage coronal restoration after root canal treatment, mesial and distal proximal contacts, tooth not acting as an abutment and non-molar tooth. In an NHS practice study of root treated lower 6s, 90% were retained at 5 years. The most important positive statistically significant factor on tooth survival was the presence of a crown (Tickle et al 2008).
- Implant fixture and supra-structure survival – prosthodontics problems become apparent between 5 and 10 years – 95% survival at 5 years and 80% after 10 years (Pjetursson et al 2012).
Deciding if a tooth is restorable
- Can we objectivise decision on tooth restorability? Tooth restorability index (Mcdonald & Setchell 2005) is useful but a long way from objectivising our decision.
- The amount, height, thickness and ferrule of remaining tooth structure is the most important factor on outcome – much more so than the type and length of post and the type of core (Creugers & Mentink 2005). Never use the presence of a post to drive decision-making – it should be the strategic worth, what you are asking of the tooth, amount of caries, remaining supra-gingival tooth tissue present, ability to isolate and make an impression as well as the risk to reward of the other options. Bitewings are useful to assess restorability as they provide a true parallel view, which allows for an accurate assessment of the amount of remaining tooth tissue coronal to the alveolar crest.
Endodontics
- Pre-operative factors that make a difference to the success of root canal treatment: presence of periapical lesion (49% lower), size of periapical lesion (14% lower for every 1 mm), presence of sinus (48% lower), presence of root perforation (56% lower) (Ng et al 2008).
- Intra-operative factors affecting success: achieving good patency (2-fold increase), canal prepared short of terminus (12% lower for every 1 mm short), long root filling (62% lower odds of success), using chlorhexidine as an irrigant (53% lower), inter-appointment swelling (47% lower) (Ng et al 2011).
- Re-treatment – can we predict what will work? The poorer the quality of the primary root filling, the easier and more predictable will be your re-treatment. You can then expect an 80% successful outcome (Ng et al 2011) if you can achieve your objectives. High-risk features to be aware of include: perforations, resorption, ledges, blockages and iatrogenic errors. Tip: For re-treatment cases, you need to get to the end of the canal very early and achieve patency.
- Don’t forget about the role of apical endodontic surgery for the re-treatment of periradicular lesions – healing rates similar if done well (Fabbro et al 2007).
Bridges
- In terms of quality of life implants, resin bonded bridges or conventional bridges are equally well received.
- Paul King’s recent (2015) study from Bristol on resin bonded bridges has confirmed very predictable outcomes with very high 10/12 year survival at 80%. The message from this study is after early failures the remaining bridges survive and perform very predictably. Also none of the patients complained of grey out and with opaque cements – this is no longer a major problem for the profession.
Implants
- Risk to reward with implants – we must be able to match the expectation of patient to reality or know when we cannot. We need to think about the final restoration at the very beginning of planning.
- Implants used to replace teeth lost due to trauma, hypodontia and caries do best (Karoussis et al 2003).
- Implant fixed dentistry aesthetics are more unpredictable when compared with tooth related aesthetics. Lip line must be carefully assessed. May need to create more bone and soft tissue to make it look tooth-like.
- Survival is good in decent bone when adequate implant length and diameter – but the implications from subsequent biological loss are potentially dire – we need to know where the risks lie.
- Risk factors for implants – IV bisphosphonates, radiotherapy, uncontrolled diabetes, immune disorder and steroids, smoking, heavy alcohol, uncontrolled periodontitis and poor OH, parafunction, anatomy, soft tissue type and form, keratinised tissue deficit, state of adjacent teeth, and past implant or graft failure. The more complex the treatment, the more likely there will be more complications and long-term problems (Poggio et al 2005). Evidence also suggests that implants placed by general practitioners are more prone to peri-implant disease than those placed by specialists.
- The periodontal patient needs to earn their implants with proof of long-term compliance to both plaque control and a maintenance programme.
- At least 50% of implants display peri-mucositis with 20% displaying peri-implantitis. As a general rule peri-implantits is likely to affect 20% of patients and peri-mucositis 40% of patients. What we do not have yet is the evidence to guide the best approach to managing this problem. Clearly changing patient behaviour – plaque control techniques will be a key part of this.
- Implant removal – Neo-Biotech implant fixture removal kit is better than using a trephine.
Concluding statements
- We must be honest and not de-value the importance of even significantly periodontally compromised teeth. Tooth preservation keeps options open and buys time.
- The final decision should be a joint decision between you and the patient. Implants certainly have a place in dentistry but we must shout loud and not allow for the loss of basic traditional prosthodontics foundation skills on the back of ‘just take it out and stick in an implant’.
Link for a similar lecture recorded at the BSRD Conference: https://www.youtube.com/watch?v=nYmvyh2atZs&autoplay=1



