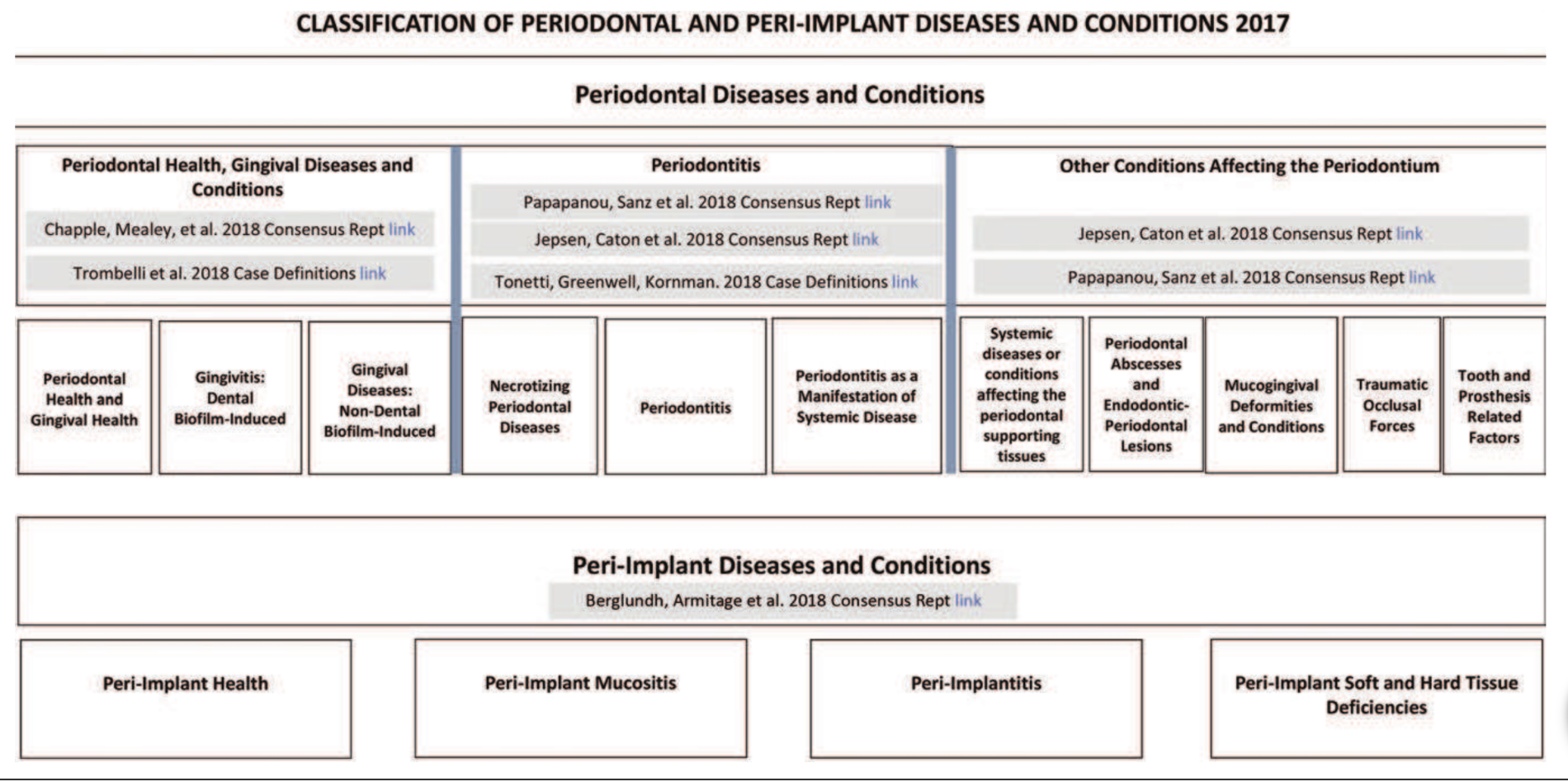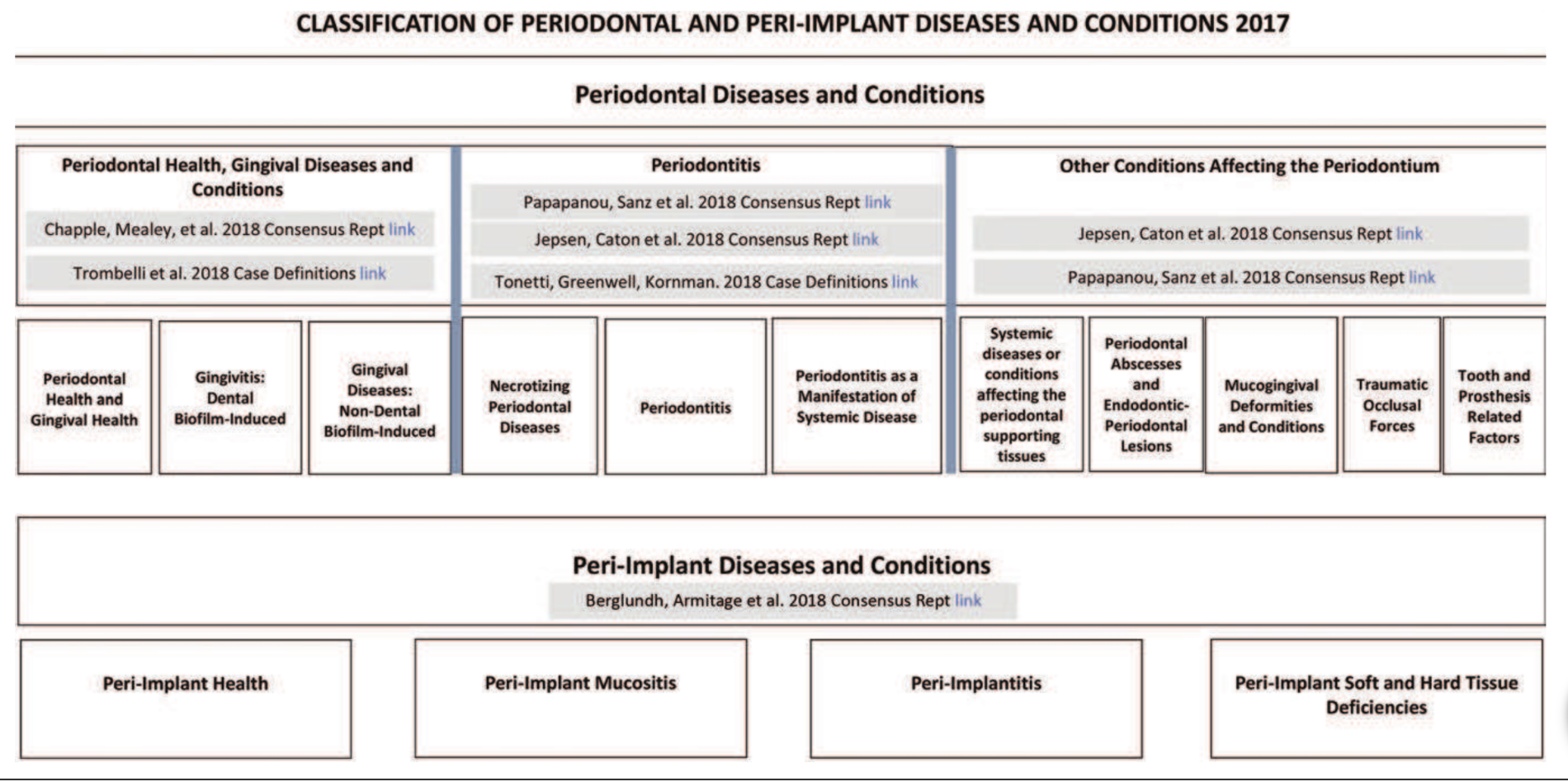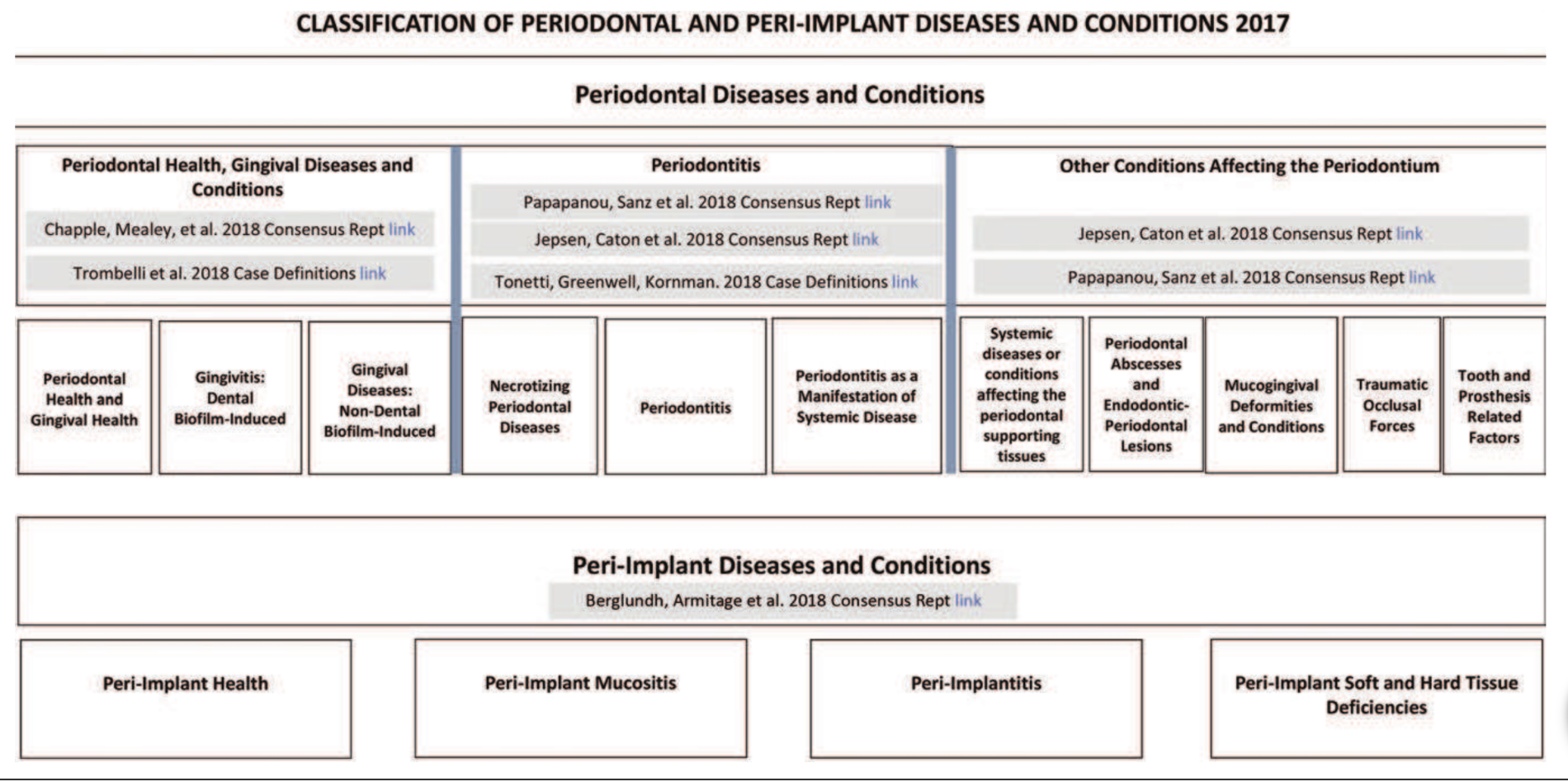
- The changes reflect the advances in scientific knowledge, including our understanding of periodontal and peri-implant diseases and the conditions that have evolved since then. “At first glance, the classification may appear complex but it is actually quite pragmatic…” Iain Chapple.
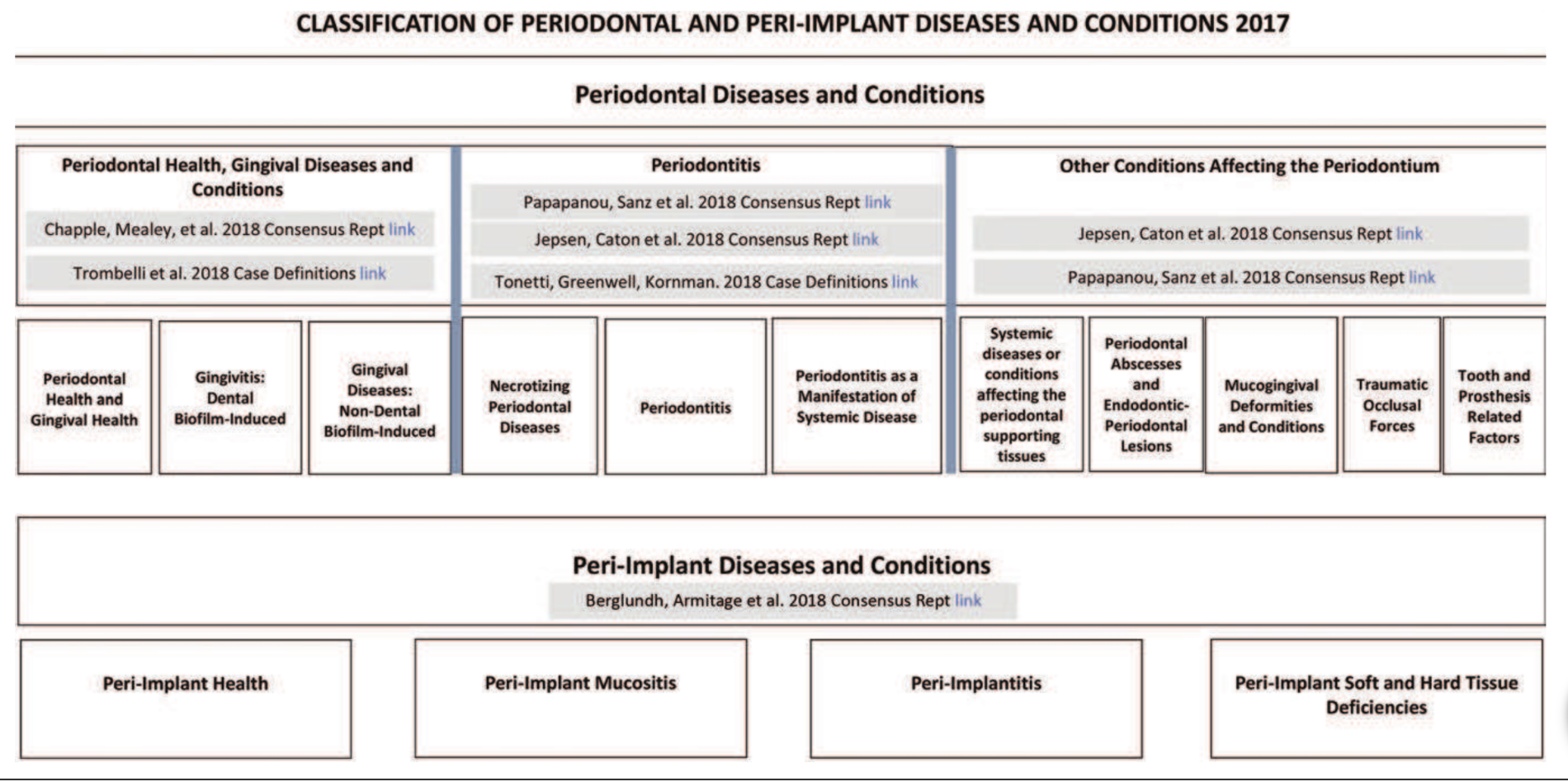
- There are four levels of periodontal health, depending on the state of the periodontium and the relative treatment outcomes:
- Pristine periodontal health, with a structurally sound and uninflamed periodontium
- Well-maintained clinical periodontal health, with a structurally and clinically sound (intact) periodontium
- Periodontal disease stability, with a reduced periodontium
- Periodontal disease remission/control, with a reduced periodontium
- Periodontal health can exist at both site and whole-mouth levels, and on an intact or a reduced periodontium. An intact periodontium is one without clinical attachment loss or bone loss, whereas a reduced periodontium may arise either in a non-periodontitis patient (e.g. patients with some forms of gingival recession or following crown-lengthening surgery) or in a patient with a history of periodontitis. Histological changes in the gingival microvasculature arise almost immediately following tooth eruption and that an inflammatory infiltrate is evident as part of normal immune surveillance, as indeed are subtle clinical signs of inflammation at isolated sites as part of “clinical health”. Therefore, pristine health is exceptional and largely seen only in textbooks. A case of clinical gingival health was established on an intact and a reduced periodontium in a non-periodontitis patient as <10% sites of bleeding on probing (BoP) and probing depths of <3 mm. The intact periodontium had no attachment loss, whereas the reduced periodontium did have evident attachment loss. In the reduced periodontium in a successfully treated periodontitis patient, health allowed probing depths up to 4mm, embracing the concept of the “closed pocket”, but there must be no BoP at any 4mm site, as this would represent the likelihood of recurrent periodontitis and indicate a need for remedial intervention. Once periodontitis is diagnosed, a patient remains a periodontitis patient for life, but may represent a case of “health” or of “gingival inflammation” at any particular time following successful therapy. In this context, the term “gingival inflammation” was employed rather than “gingivitis”. Although technically they mean the same thing, it was felt that one could not have a periodontitis patient who also has a diagnosis of gingivitis. However, a periodontitis patient may have sites of gingival inflammation at probing depths of <3mm following treatment, but such patients may not require root-surface debridement for recurrent periodontitis, but rather need oral-hygiene reinforcement and plaque removal to manage localised gingival inflammation.
- Gingivitis was categorised simply as gingivitis on an intact or a reduced periodontium
and definitions were made of predisposing factors (local risk factors) that lead to increased plaque accumulation and of modifying factors (systemic risk factors) that alter the nature of the immune-inflammatory response to plaque.
- The non-plaque-induced gingival conditions and lesions were stratified into eight groups, differentiating them from non-plaque-induced periodontal conditions: a) genetic/ developmental; b) specific infections; c) inflammatory/ immune; d) reactive; e) neoplasms; f) endocrine, nutritional and metabolic, g) traumatic; h) pigmentation.
- It was concluded that there was a lack of evidence for the distinction between “chronic” and “aggressive” periodontitis. The new classification is based on four stages and three grades. Stages are assessed in terms of extent and distribution as: localised, generalised, and molar-incisor distribution. By combining these defined stages and grades, we can individualise the modalities and sequences of existing therapies, which will allow us to better assess their results.
- Stage 1 – Initial periodontitis – a very incipient periodontitis with clinical attachment loss and bone loss limited to the most coronal portion of the root. In this stage, patients do not present periodontal pockets and they have not suffered tooth loss caused by periodontitis.
- Stage 2 – Moderate periodontitis – periodontal destruction affects the coronal third of the root and is characterised by
the presence of moderate periodontal pockets (<5mm) and the patient has not yet lost teeth because of periodontitis.
- Stage 3 – Severe periodontitis with potential for additional tooth loss – A limited amount of tooth loss has usually already occurred and the presence of furcation and intrabony lesions is common. All these aspects make the treatment of this stage complex and surgical interventions are usually needed.
- Stage 4 – Severe periodontitis with potential for loss of the dentition – increases the severity and complexity of the previous stage by an increased tooth loss (>5 teeth) and the presence of masticatory dysfunction, which usually requires a complex multidisciplinary treatment beyond the periodontal therapy.
- Grade A – The rate of progression is low and the patient does not have risk factors.
- Grade B – The expected progression.
- Grade C – The patient has evident risk factors and there is a high risk of periodontal progression.
- Periodontal manifestations of systemic diseases and conditions: There are rare systemic disorders, such as Papillon–Lefèvre syndrome, that result in the early presentation of severe periodontitis. Such conditions are grouped as Periodontitis as a manifestation of systemic disease. Their classification is based on the primary systemic disease. Other systemic conditions, such as neoplastic diseases, can affect the periodontal tissues independently of biofilm- induced inflammation. They are also classified based on the primary systemic disease and are now grouped as Systemic diseases or conditions affecting the periodontal supporting tissues. On the other hand, there are more common systemic diseases – i.e. diabetes mellitus – that are important modifiers of the course of periodontitis. However, diabetes-associated periodontitis should not be regarded as a distinct diagnosis – diabetes is now included in the new clinical classification of periodontitis as a descriptor in the grading process. In a similar way, smoking – now regarded as nicotine dependence and as a chronic relapsing medical disorder with major negative effects on the periodontium – is now also included in the clinical diagnosis of periodontitis as a descriptor.
- Mucogingival conditions: In the context of mucogingival conditions, the importance of the gingival phenotype, including gingival thickness and width, is now recognised and a new classification for gingival recessions has been introduced. This combines clinical parameters such as the gingival phenotype, the interproximal attachment loss, and the characteristics of the exposed root surface.
- Occlusal trauma and traumatic occlusal forces: Traumatic occlusal force, which replaces the term “excessive occlusal force”, is any occlusal force that results in injury to teeth (such as excessive wear or fracture) and/or to the periodontal attachment apparatus. Occlusal trauma is a histological term to describe the injury of the periodontal attachment apparatus. There is no evidence from human studies that traumatic occlusal forces lead to periodontal attachment loss, non-carious cervical lesions, or gingival recessions. Traumatic occlusal forces lead to adaptive mobility in teeth with normal support, and to progressive mobility in teeth with reduced support, usually requiring splinting.
- Prosthesis and tooth-related factors: This section is expanded in the new classification. The term biologic width is replaced by supracrestal tissue attachment, consisting of junctional epithelium and supracrestal connective tissue. Evidence from human studies indicates that infringement of restorative margins within the supracrestal connective tissue attachment is associated with inflammation and/or loss of periodontal supporting tissue. However, it is not clear whether these negative effects are caused by dental biofilm, trauma, toxicity of dental materials, or a combination of these factors. On the other hand, certain tooth- related anatomical factors – such as enamel projections/ pearls, root fractures, and proximity – are related to dental-biofilm-induced gingival inflammation and loss of periodontal supporting tissues.
- Peri-implant health: Characterised by the absence of clinical signs of inflammation,including bleeding on probing, no increase in probing depth compared to previous examinations and no bone loss beyond crestal bone-level changes resulting from initial bone remodelling. It is not possible, however, to define a range of probing depths compatible with health. In addition, peri-implant health can exist around implants with reduced bone support.
- Peri-implant mucositis: An inflammatory lesion of the soft tissues surrounding an endosseous implant in the absence of loss of supporting bone. The lesion is located lateral to the junctional/pocket epithelium but does not extend into the supracrestal connective tissue zone, “apical” of the junctional/pocket epithelium. The main clinical characteristic of peri-implant mucositis is bleeding on gentle probing, while other clinical signs of inflammation may also occur. There is strong evidence that plaque is the aetiological factor for peri-implant mucositis. The case definition of peri-implant mucositis includes: bleeding and/or suppuration on gentle probing and no bone loss beyond crestal- bone level changes resulting from initial bone remodelling.
- Peri-implantitis: Plaque-associated pathological condition occurring in tissues around dental implants, characterised by inflammation in the peri-implant mucosa and loss of supporting bone. Peri-implantitis lesions extend apical of the junctional/pocket epithelium and are larger than those at peri-implant mucositis sites. Peri-implantitis sites exhibit clinical signs of inflammation including bleeding on probing and/or suppuration, increased probing depths in addition to radiographic bone loss. In the absence of previous examination data, diagnosis of peri-implantitis can be based on the combination of bleeding and/or suppuration on gentle probing, probing depths of >6mm and bone levels >3mm apical of the most coronal portion of the intra-osseous part of the implant.
- Hard- and soft-tissue deficiencies: Healing following tooth loss leads to diminished dimensions of the alveolar process/ridge that result in hard- and soft- tissue deficiencies. Ridge deficiencies can occur at sites associated with severe loss of periodontal support, extraction trauma, endodontic infections, root fractures, thin buccal bone plates, poor tooth position, injury, and pneumatisation of the maxillary sinuses.
Periodontology
Recent post
June 29, 2023
Pink Aesthetics...
Read more
General Dental,Periodontology
June 26, 2022
10 Key Points from EuroPerio10...
Read more
Periodontology,Reena's Notes
June 11, 2021
Working as a hygienist or therapist...
Read more
General Dental,Periodontology