Home/Articles
/ General Dental /
10 Key Points on the Perio-Restorative Interface with Miss Ulpee Darbar
June 22, 2021
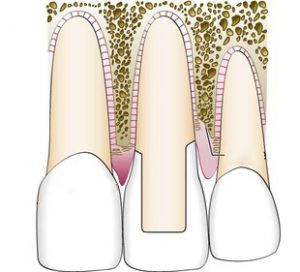
- The periodontal-restorative interface is that between the tooth and the marginal gingival tissues. Any disruption to the area is likely to lead to inflammation. Any inflammation in this area is likely to compromise the outcome of the restorative procedure. Understanding the relationship between this interface will lead to improved predictability and outcomes of restorative treatment. Examples of restorative factors to consider include: location of margins, marginal adaptation, contact areas, design of fixed/removable prostheses and iatrogenic damage.
- One particularly important concept relating to this is that of the biologic width i.e. the connective tissue and epithelial attachment (Gargiulo 1961). If this is encroached during restorative procedures it can lead to gingival recession (in thin biotypes) or chronic inflammation (in thick biotypes).
- The concept of altered passive eruption needs to be understood in cases of gingival tissue excess particularly when considering restorative procedures. The different types and subtypes are also important to understand.
- In altered passive eruption, the periodontal-restorative interface is different and any planned restorative procedure needs to undertaken with this in mind. Passive eruption is where the gingival margin migrates in an apical direction with gradual exposure of the crown of the tooth and final stable localisation of the dentogingival unit close to/at the cervical level. Altered passive eruption is when the marginal gingivae is coronally malpositioned and does not approximate to the CEJ (Goldman & Cohen 1965). Prevalence ranges from 7-14% and it is more common in patients with thick flat gingival tissue biotype (Garber & Salama 1996). It can be classified into categories (Coslet et al 1977): Type 1A: wider band of keratinised tissue, normal level of osseous crest; Type 1B: wider band of keratinised tissue osseous crest at CEJ; Type 2A: smaller band of keratinised tissue, normal level of osseous crest; Type 2B: smaller band of KT, osseous crest at CEJ. The treatment options will depend on the type: Type 1A – gingivectomy, apically repositioned flap; Type 1B – gingivectomy, osseous recontouring, apically repositioned flap; Type 2A – apically repositioned flap; Type 2B – osseous recontouring, apically repositioned flap. If this condition is not assessed and diagnosed correctly, the wrong procedure could create challenges e.g. either inflammation around the restorations in thick biotypes or recession in thin biotypes.
- Crown lengthening surgery is an option that can be considered to minimise the risk of violating the biologic width. When considering crown lengthening, the rationale for the surgery must be considered and a detailed pre-operative assessment undertaken which should include an assessment of the gingival tissue biotype, the objective of the surgery along with appropriate good quality radiographs. In some cases e.g. tooth wear, sensibility testing may be necessary of the teeth involved prior to the surgery and often a diagnostic wax up will aid the planning and also discussion with the patient.
- The planning will help with ensuring a risk assessed approach is used. Your patients MUST be warned about sensitivity, longer clinical crowns and open embrasure spaces (black triangles) that may create aesthetic concern.
- It is important to consider the gingival tissue biotype when carrying out crown lengthening surgery. Studies show that after surgery, marginal tissues have a tendency to grow in a coronal direction from the level defined at surgery. The pattern of coronal displacement is more pronounced in patients with “thick” tissue biotype but also appears to be influenced by individual variation. The amount of rebound also seems to be related to the position of the flap relative to the alveolar crest at suturing (Deas 2004). Therefore for patients with thick biotypes, overcorrect to allow for some rebound. 6-8 weeks following surgery, the provisional crown should be placed to allow for maturation before the definitive crown.
- The biologic width is usually re-established to its original vertical dimension by 6 months (Lanning et al 2003).
- When considering crown lengthening surgery for patients with short clinical crown height, if the risk of undertaking the surgery is going to compromise the tooth, the alternative options to crown lengthening surgery e.g. orthodontic extrusion of teeth and reorganising the occlusion should be considered.
- A coronal gingival margin position, known often as gingival tissue excess, is common following orthodontic treatment. Resist the urge to surgically correct this immediately as the tissues will remodel for at least 3-6 months post treatment. At reassessment the final gingival margin can be assessed with a need for surgical intervention.
These notes were derived from a webinar produced by the British Society of Periodontology. Further resources can be found at: www.bsperio.org.uk.
Learn more by reading some of our other articles here. 22